Vascular Access Planning
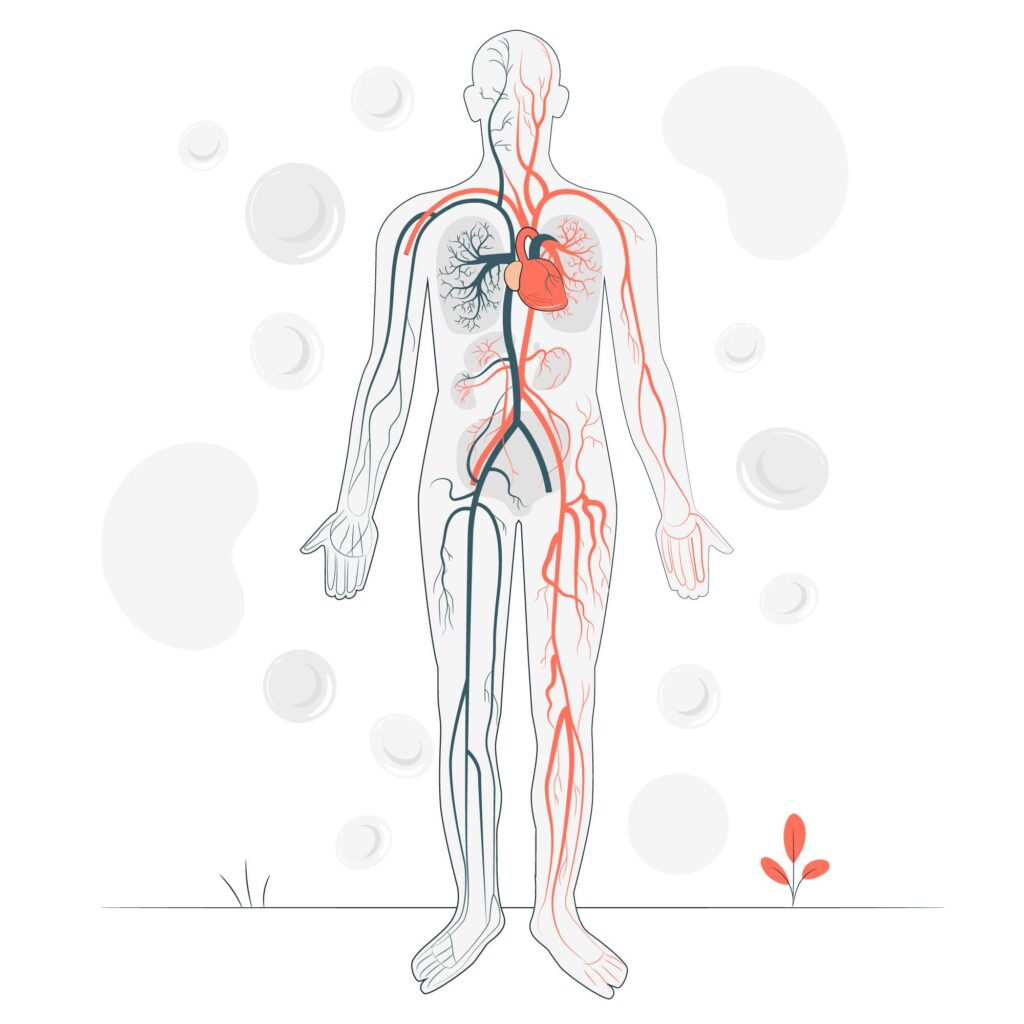
Vascular access planning is a critical aspect of managing patients requiring hemodialysis for end-stage kidney disease (ESKD). It involves the creation and maintenance of access points that allow for repeated access to the bloodstream for dialysis treatments.
Types of Vascular Access
There are three main types of vascular access used for hemodialysis:
Arteriovenous Fistula (AVF):
- Surgical Creation: Involves surgically connecting an artery to a nearby vein, typically in the arm.
- Preferred Option: Considered the gold standard due to lower infection and complication rates, and longer durability.
- Maturation Period: Requires time to mature and develop adequate blood flow before it can be used for dialysis.
Arteriovenous Graft (AVG):
- Synthetic Tube: Uses a synthetic tube to connect an artery and a vein, usually in cases where an AVF cannot be created.
- Shorter Maturation: Can be used sooner after placement compared to AVFs but has a higher risk of infection and thrombosis.
Central Venous Catheter (CVC):
- Temporary Option: Insertion of a catheter into a large vein in the neck, chest, or groin for immediate dialysis access.
- Higher Complication Risk: Associated with higher infection rates and long-term complications like vein narrowing (stenosis) and thrombosis.
Planning and Maintenance
Effective vascular access planning involves:
- Assessment: Evaluating the patient’s vascular anatomy and considering factors such as previous access history, comorbidities, and expected duration of dialysis.
- Selection: Choosing the most suitable type of vascular access based on individual patient factors and preferences.
- Monitoring: Regular monitoring of access function, blood flow rates, and complications to ensure optimal dialysis efficiency and minimize risks.
Patient Education
Dr. Tanish Dhir emphasizes the importance of patient education in vascular access care:
- Self-Care: Teaching patients how to monitor their access site, recognize signs of complications, and maintain good hygiene practices.
- Empowerment: Encouraging patients to actively participate in their care and adhere to recommended follow-up appointments and maintenance protocols.
